Navigate memory care Howell. Discover top facilities, costs, and tips to select the perfect senior living for your loved one.

The Long Haul: A Guide to Alzheimer’s and Dementia Care Options
Alzheimer’s long term care: 6 Essential Options
Why Alzheimer’s long term care Matters More Than You Think
Alzheimer’s long term care provides specialized support when memory loss and cognitive decline make it unsafe to remain at home. The main options include:
- Memory Care Units – Secure facilities with staff trained in dementia care, offering 24/7 supervision and specialized programming.
- Assisted Living with Dementia Support – Communities providing help with daily activities plus some memory care services.
- Nursing Homes – For those needing round-the-clock medical care alongside dementia support.
- Adult Day Centers – Part-time care providing activities and supervision while family caregivers work.
- In-Home Care Services – Professional caregivers who come to your loved one’s home.
The time to consider long-term care often comes when safety is at risk due to wandering, when behaviors become unmanageable, or when the weight of 24/7 caregiving impacts your own health.
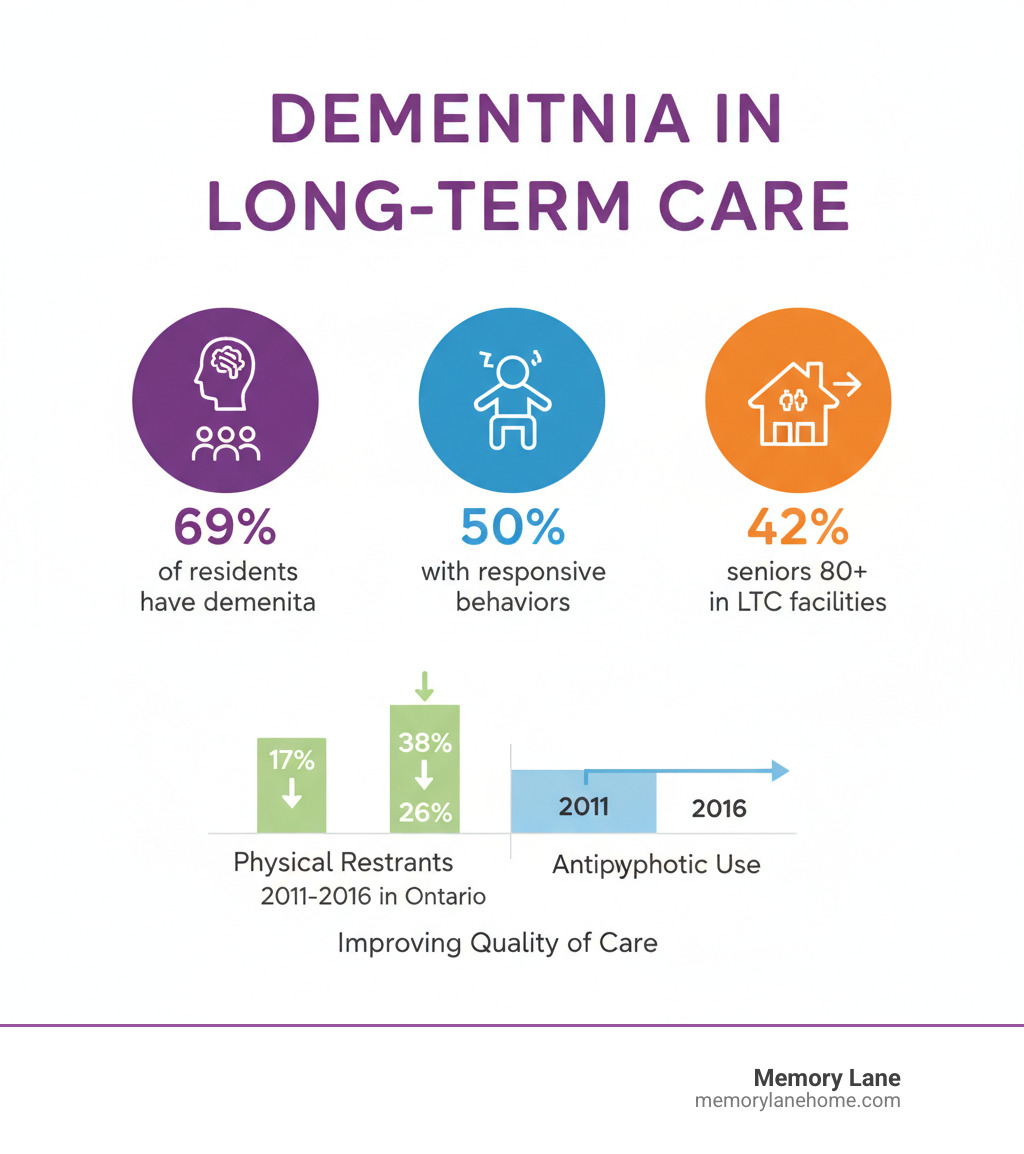
Statistics show that as Alzheimer’s progresses, most families eventually need professional support. In 2015-2016, 69% of residents in long-term care homes had dementia. For those 80 and older with dementia, 42% live in long-term care facilities.
Making this decision isn’t a failure; it’s choosing the best possible care for your loved one. The guilt and stress you may feel are normal parts of this transition.
I’m Jason Setsuda, CFO of Memory Lane Assisted Living and a Medical Director with over 10 years of experience. I’ve guided countless families in finding quality Alzheimer’s long term care. This guide will help you understand your options, know when to seek help, and make the right decision for your family.
Recognizing the Signs: When to Consider Long-Term Care
Many caregivers eventually ask themselves, “Can I keep doing this?” The question often follows a difficult night or a frightening incident, becoming more persistent over time.
Deciding to move a loved one into Alzheimer’s long term care is one of life’s hardest decisions, often following years of home care. This decision isn’t about giving up; it’s about recognizing when your loved one’s needs exceed what can be safely provided at home.
When caregiver stress becomes burnout, it’s a clear sign a change is needed. The 24/7 demands of Alzheimer’s care can lead to chronic exhaustion, irritability, and depression. You might neglect your own health and social life. These are not signs of weakness but warnings of burnout. As the Alzheimer Society reminds us, you must “balance [the needs of the person you’re caring for] with your own well being. You shouldn’t have to do it all alone.”
Safety concerns are often the tipping point. Incidents like wandering, leaving the stove on, or frequent falls can escalate quickly. A specialized facility provides a secure environment designed to prevent these dangers.
Aggressive or challenging behaviors can emerge as Alzheimer’s progresses, such as hitting, shouting, or resisting care. In 2015–2016, 50% of residents with dementia in long-term care experienced these behaviors. Trained staff can manage these situations safely, which can be frightening and dangerous for family caregivers.
The struggle with daily activities is another sign. When your loved one needs extensive help to bathe, dress, eat, or use the bathroom, the physical demands can become overwhelming. This level of care often requires round-the-clock professional support.
Staying home can lead to isolation for both you and your loved one. As caregiving consumes your time, social connections fade. Specialized care settings provide structured activities and social interaction that can combat this isolation.
As the Cleveland Clinic notes, “the needs of individuals with Alzheimer’s change significantly throughout the illness.” This requires constant reassessment. Statistics reflect this: about one-third of seniors under 80 with dementia live in long-term care, rising to 42% for those 80 and older.
This progression is natural. Seeking professional Alzheimer’s long term care is a loving choice to ensure your family member gets the support they need, allowing you to transition from an exhausted caregiver to a supportive advocate.
Exploring Alzheimer’s Long-Term Care Options
There is no single solution for Alzheimer’s long term care. The right choice depends on your loved one’s stage of illness, their support needs, and your family’s comfort. The goal is to find a place where they are safe, engaged, and treated with dignity.

Many families move through a continuum of care, starting with in-home support and later transitioning to assisted living or memory care. Some communities offer multiple levels of care on one campus, allowing residents to age in place as their needs change, which provides peace of mind.
Types of Care Settings
Let’s walk through the main residential care settings for people with Alzheimer’s and related dementias.
Assisted living facilities are a middle ground, offering help with daily activities like bathing, dressing, and medication reminders. They provide meals, social activities, and some health services. This option is for those who need support but not 24/7 medical care. Be aware that regulations and dementia training vary by state and facility.
Memory care units are purpose-built for people with dementia. They can be standalone facilities or dedicated wings. Key features include secure layouts to prevent wandering, staff with specialized dementia training, cognitive engagement activities, and 24/7 supervision. At Memory Lane, we focus exclusively on this personalized, compassionate care in a secure setting.
Group homes are a more intimate option, with a few residents living with caregivers. The smaller scale feels more like home and allows for more one-on-one attention. However, regulatory oversight may be less stringent than in larger facilities, so thorough research is essential.
Nursing homes provide the highest level of medical care with 24/7 skilled nursing staff. This is the right choice for those with complex medical needs or who require extensive assistance. These facilities are heavily regulated and often include specialized dementia units.
Here’s how assisted living and memory care compare on key features:
| Feature | Assisted Living | Memory Care |
|---|---|---|
| Level of Care | Assistance with ADLs (bathing, dressing, medication reminders), general supervision. | 24/7 supervision, specialized dementia care, structured routines, improved safety. |
| Typical Resident | Needs some help with daily tasks, generally independent. | Diagnosed with Alzheimer’s or other dementias, may wander, behavioral challenges. |
| Environment | Apartment-like, less secure, more freedom of movement. | Secure, easy-to-steer layouts, often specific design elements to reduce confusion. |
| Staff Training | General elder care training, some dementia awareness. | Extensive, specialized training in dementia care, managing responsive behaviors. |
| Activities | General social activities, outings. | Memory-stimulating activities, music therapy, sensory engagement, custom to cognitive levels. |
| Cost | National average $70,800 per year (basic services). | Generally higher than assisted living, average $4,000-$7,000 per month. |
In-Home and Community-Based Alternatives
Residential facilities aren’t the only option, especially in earlier stages. In-home care services and community programs can help your loved one stay at home longer.
In-home care services bring professional help to your home, from aides for personal care to skilled nurses for medical needs. It’s a common starting point for families needing to fill caregiving gaps.
Adult day centers provide a supervised setting with dementia-specific activities during the day. This gives caregivers a break and helps combat the resident’s social isolation.
Respite care offers short-term stays (e.g., a week or two) in facilities, giving family caregivers a necessary break to rest or handle other responsibilities. Using respite care is essential for your own well-being.
Home safety modifications can also extend the time someone can live at home safely. As the Cleveland Clinic notes, a home assessment can “reduce the risk of falls and limit the potential for wandering.” Simple changes like removing rugs, installing grab bars, and improving lighting make a big difference.
Finding local dementia resources and programs is easier than you might think. The Eldercare Locator is a great starting point (you can also call 800-677-1116). For broader information about housing options and services, visit LongTermCare.gov. Your local Area Agency on Aging can connect you with programs right in your community.
The key is to match the level of care to current needs while anticipating future ones. This is an ongoing conversation, not a one-time decision.
How to Choose the Right Facility: A Detailed Checklist
Choosing a care facility is overwhelming. You’re deciding where your loved one will live and who will care for them. This decision requires time, observation, and asking many questions.

Visit several communities, including unannounced drop-ins at different times. Mealtimes are revealing: observe staff-resident interactions, the food quality, and the overall atmosphere.
Talk to current residents and their families. They offer a candid perspective on life in the facility.
Before visiting, do your homework. Ask for the latest survey or inspection report. Use online tools like Medicare’s Nursing Home Compare, the broader Medicare Care Compare tool, and the Joint Commission’s Quality Check to research and compare facilities.
What to Look for in Alzheimer’s Long-Term Care Staffing
The quality of an Alzheimer’s long term care facility depends on its staff. A beautiful building is meaningless without properly trained, compassionate caregivers.
Staff-to-resident ratios indicate the level of individual attention. Ask for day and night shift numbers; a lower ratio is better, especially overnight when wandering risks are higher.
Dementia-specific training is crucial. Caregivers need specialized knowledge of how Alzheimer’s affects behavior and communication. Ask about the extent and frequency of this training. At Memory Lane, our staff receive continuous, specialized training because a deep understanding of dementia is vital for quality care.
Check staff turnover rates. High turnover is disruptive for residents with dementia who rely on familiar faces. Low turnover suggests a positive work environment and better continuity of care.
Observe how staff interact with residents. Do they show genuine warmth and respect? Do they make eye contact and speak to residents directly? These small interactions reveal the facility’s culture.
Inquire about their approach to handling challenging behaviors. A good facility will focus on understanding triggers and using non-pharmacological interventions (person-centered care) rather than defaulting to medication or restraints.
Medical staff availability is crucial. Ask how often doctors and nurses are on-site and if a registered nurse is available 24/7 for prompt responses to health changes.
Care has improved significantly. For example, in Ontario between 2011-2015, physical restraint use in long-term care dropped from 17% to 7%, and potentially inappropriate antipsychotic use fell from 38% to 26%.
However, challenges remain. In 2015-2016, residents with dementia were still more likely to receive antipsychotics without a psychosis diagnosis (27% vs. 11%) and be physically restrained (9% vs. 3%). This highlights the importance of a person-centered care philosophy and the need to ask direct questions about these practices.
Programs, Environment, and Resident Care
Beyond the people who provide care, the physical environment and daily programming shape your loved one’s quality of life.
Review the activity calendar. It should offer a variety of events, including on weekends and evenings. Ensure activities are appropriate for dementia, such as music therapy, art, and sensory engagement, custom to different cognitive levels.
The physical environment must be safe and comfortable. Look for secure indoor and outdoor areas, easy-to-steer layouts, and monitored exits to prevent wandering. Good lighting and thoughtful design can reduce confusion and provide comfort.
Cleanliness is non-negotiable. Walk through common areas and pay attention to any odors. A well-maintained facility shows respect for its residents.
Visit during mealtime. Is the food appetizing and the dining room pleasant? Do they accommodate special diets and offer flexibility? Observe how staff patiently and respectfully assist residents who need help eating.
Personal care should preserve dignity. Are residents well-groomed? Does the staff respect individual routines and privacy?
Ask about fall rates and prevention strategies. In 2015-2016, 16% of residents with dementia fell, compared to 11% of those without. How does the facility prevent and respond to falls?
Revisit the topic of restraints and antipsychotics. A quality facility will prioritize non-pharmacological interventions to address residents’ underlying needs.
Consider how families are involved. Are you treated as a partner in care planning? How is communication handled? Are visiting hours flexible? Your role shifts to being an advocate on the care team.
Key Questions for Your Facility Tour
Bring this list with you when you visit facilities:
- What are your staff-to-resident ratios (day and night)?
- What specific, ongoing dementia training do staff receive?
- How do you handle challenging behaviors? What is your policy on restraints and antipsychotics?
- Can I see your latest state inspection report?
- What is a typical day like for a resident? Can I see an activity calendar?
- How are families involved in care planning and updated on a resident’s condition?
- What is your policy on “aging in place” if care needs increase?
- What security measures prevent wandering?
- How do you handle dining, special diets, and preferences?
- What does the monthly fee include, and what costs extra?
- What is your discharge policy?
- Are private spaces available for family visits?
- How do you ensure personal care is dignified and respects preferences?
- What is your fall prevention program and recent fall rate?
Understanding the Costs of Alzheimer’s Long-Term Care
The financial reality of Alzheimer’s long term care weighs heavily on families. Understanding the costs upfront is crucial for planning and making informed decisions.

The costs are substantial. According to Genworth’s Cost of Care Survey, basic assisted living averages $70,800 per year. Nursing home care averages $127,750 annually for a private room or $111,324 for a semi-private room.
Memory care costs more than standard assisted living due to specialized staff and services. Expect to pay between $4,000 and $7,000 per month, depending on location and level of care.
The monthly fee typically includes housing, meals, personal care assistance, activities, and 24/7 supervision.
Some services, like specialized therapies or one-on-one care, may cost extra. Always ask for a detailed breakdown of what’s included versus what incurs additional charges.
Financial Assistance for Alzheimer’s Long-Term Care
The good news is that financial assistance is available, though navigating the options can be complex.
Many families use private pay (savings, pensions). If your loved one has long-term care insurance, review the policy carefully to understand what facilities and services it covers, as this can significantly reduce out-of-pocket costs.
A common misconception is that Medicare covers long-term care. Medicare does not cover long-term residential care. It only covers short-term skilled nursing care after a hospital stay, not the ongoing custodial care in assisted living or memory care.
Medicaid can cover long-term care costs for those who meet strict, state-specific income and asset limits. If you anticipate needing Medicaid, consult an elder care lawyer early to steer the rules and plan accordingly.
If your loved one is a veteran, investigate Veterans benefits. The Aid and Attendance benefit can provide financial assistance for those needing help with daily activities.
The U.S. Department of Health and Human Services’ website offers helpful information about costs and payment options for various housing choices.
An elder care attorney can be invaluable during this process. They help families understand complex regulations, develop financial strategies, and apply for benefits.
Navigating the Move: Preparing for and Managing the Transition
Moving your loved one into Alzheimer’s long term care is incredibly difficult. It’s normal to feel a mix of guilt, sadness, and relief. Acknowledge that these complex feelings are valid.
Prepare emotionally by reminding yourself you are ensuring specialized care, not abandoning them. Talk to friends, family, or a support group like ALZConnected. The Alzheimer’s Association 24/7 Helpline (800.272.3900) also offers support.
Involve your loved one in downsizing and packing as much as possible to give them a sense of control. Focus on bringing familiar, cherished items like a favorite armchair, photo albums, or a quilt. These items are anchors to their identity.
Create a familiar space in their new room to ease the adjustment. Arrange furniture intuitively and display personal items like photos and blankets. At Memory Lane, we encourage personalization because we know it transforms a room into a comforting home.
Plan your move-in day strategy with the facility staff. The best approach varies for each person. Keep the day calm and positive, framing it as a move to a “new home” rather than focusing on what’s left behind.
Adjustment takes patience. The first few weeks may be difficult, with confusion or withdrawal. This is normal. Visit regularly, but follow staff advice on frequency. Bring familiar activities, like photo albums or music, to share during visits.
Your role as a caregiver transforms. You become their advocate and champion. Freed from the physical demands of care, you can focus on your emotional connection, which can deepen your relationship.
Build a partnership with the facility staff. Share stories and information about your loved one’s life and preferences to help them provide person-centered care. Open, respectful communication is key; they are your partners.
You don’t have to steer this transition alone. The Alzheimer’s Association Community Resource Finder can help you locate local dementia resources and support services. If concerns arise about care, the National Long-Term Care Ombudsman Resource Center provides advocates who can help resolve issues.
Choosing professional Alzheimer’s long term care isn’t the end of your caregiving journey—it’s the beginning of a new chapter where your loved one receives specialized support while you maintain the loving connection that matters most.
Conclusion
Seeking Alzheimer’s long term care is a difficult but courageous decision. It begins with recognizing your loved one needs more support than you can provide alone, prioritizing their safety and quality of life.
This guide has covered the signs it’s time for professional care, from caregiver burnout to safety concerns. We’ve explored the spectrum of options, including memory care, assisted living, and in-home services, to help you find the right fit for your loved one’s needs.
We provided a roadmap for evaluating facilities on staffing, environment, and care philosophy. We also covered the financial realities and the emotional weight of this transition for everyone involved.
Quality Alzheimer’s long term care is about more than just supervision. It’s about specialized care that sees the person behind the diagnosis, creating opportunities for engagement, dignity, and joy. It’s about trained staff who can calm anxiety and redirect confusion with compassion.
The right care setting provides your loved one with 24/7 support while allowing you to transition from an exhausted caregiver to a present, supportive advocate. This gives you space to care for yourself and focus on your relationship.
At Memory Lane, we understand this deeply. Our community is built on personalized care plans, engaging activities, and a secure environment where residents can thrive. We treat every resident like family.
If you are in the Ann Arbor, Ypsilanti, or Saline areas, we invite you to see what specialized memory care looks like when done right. Learn more about our specialized memory care in Ann Arbor, Michigan. We are here to answer your questions and support you on this journey.


