Navigate memory care Delray FL with our guide. Discover costs, quality, specialized programs & ensure safe, compassionate support.

Finding Your Fit: A Comprehensive Look at Dementia Care and Support Programs
Dementia Care Options: 4 Confident Choices 2025
Why Understanding Your Dementia Care Options Matters Now
When a loved one receives a dementia diagnosis, families face urgent questions about safety, support, and the future. Understanding the full spectrum of dementia care options is crucial for planning ahead and avoiding crisis-driven decisions. As the disease progresses, needs will change, and what works today may need adjustment tomorrow. This guide will help you steer those choices.
Quick Overview of Main Care Options:
- In-Home Care – Professional caregivers assist with daily tasks while your loved one stays home.
- Adult Day Centers – Structured daytime programs offering activities and social engagement.
- Assisted Living – Residential communities with help for daily activities and medication management.
- Memory Care – Specialized secure facilities designed specifically for dementia patients.
- Nursing Homes – 24/7 medical care and supervision for complex health needs.
- Hospice Care – Comfort-focused support in the final stages of life.
As Jason Setsuda, CFO of Memory Lane Assisted Living and a board-certified Emergency Medicine Physician, I’ve seen that informed families make better decisions and experience less stress. My experience as a Medical Director has shown me the importance of finding the right fit for each unique situation.
First Steps: Assessing Your Loved One’s Unique Needs
Before choosing from the available dementia care options, you must understand your loved one’s specific needs. This assessment goes beyond the diagnosis to include their daily life, safety, and well-being.
Start by evaluating their ability to perform activities of daily living (ADLs), such as bathing, dressing, and eating. As dementia progresses, these tasks become challenging. Safety is another critical concern. Assess the home for risks like an unattended stove, potential falls, or incorrect medication use. Determine the level of supervision needed, from occasional help to 24-hour monitoring.
Consider their medical requirements beyond dementia, such as diabetes or heart disease, and how multiple medications are managed. Also, evaluate their need for social engagement, as isolation can worsen cognitive decline. Whenever possible, involve the person with dementia in these discussions, especially in the early stages, to preserve their dignity and sense of control.
Finally, create a care team by involving family, friends, and professionals. Sharing responsibilities for appointments, finances, and companionship prevents any single person from burning out.
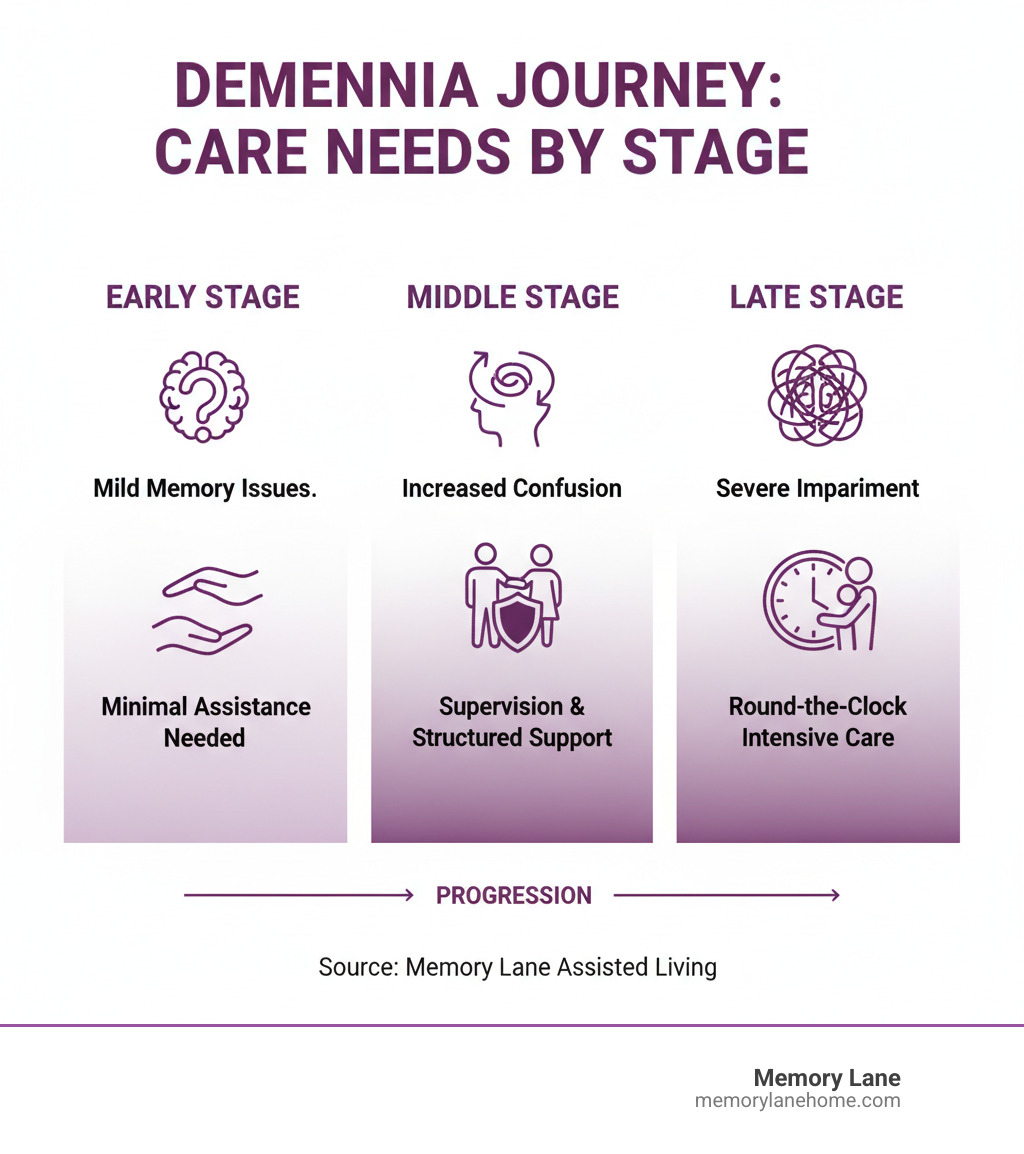
How Care Needs Change Through the Stages of Dementia
Dementia is a progressive disease, and care needs evolve over time. Understanding these stages helps you plan effectively.
Early-Stage Dementia: Individuals may forget recent events or struggle with complex tasks like managing finances but can often live independently. Support focuses on establishing routines and adapting activities for people with Alzheimer’s to maintain engagement and independence.
Middle-Stage Dementia: Confusion and memory loss deepen, and safety becomes a primary concern. Individuals need hands-on help with personal care, and wandering may become an issue, often requiring 24-hour supervision. Communication becomes more difficult, and families may start considering residential care options.
Late-Stage Dementia: Individuals become fully dependent on others for all aspects of care. They may lose the ability to speak or recognize family. Care becomes intensive, focusing on comfort, dignity, and managing physical complications like difficulty swallowing.
The Role of Medical Professionals in Care Planning
A thorough medical assessment is the most important first step. It provides a clear diagnosis and foundation for your care plan.
- Primary Care Physician: Your first stop for evaluating symptoms and coordinating referrals.
- Neurologists: Specialize in brain disorders and can pinpoint the specific type of dementia (e.g., Alzheimer’s, Vascular, Lewy body).
- Geriatrician: An expert in the health needs of older adults, managing how dementia interacts with other conditions.
- Geriatric Care Managers: Act as guides, helping families steer services and create a comprehensive care plan.
The diagnostic process includes a comprehensive assessment with cognitive testing, a physical exam, and a review of medical history. Brain scans (CT, MRI) and lab tests may be used to rule out other conditions. This evaluation provides the clarity needed to make informed decisions about the right dementia care options.
Exploring the Spectrum of Dementia Care Options
Finding the right dementia care options means matching services to your loved one’s current needs while remaining flexible for the future. The best plan supports both the person with dementia and their caregivers.
Option 1: In-Home Care and Support
Staying in a familiar environment can reduce confusion and anxiety for a person with dementia. In-home care brings support to their doorstep, ranging from companionship and personal care assistance (bathing, dressing) to skilled nursing for medical tasks. Home health aides can help with meal preparation, light housekeeping, and errands. While this option promotes independence, the need for round-the-clock supervision in later stages can become emotionally, physically, and financially challenging for families.
Option 2: Community and Day Programs
Adult day centers provide a bridge between independence and residential care. They offer structured activities, socialization, and therapeutic programs in a safe environment during the day, allowing your loved one to return home in the evening. For caregivers, these programs offer vital respite to work, rest, or manage other responsibilities.
Option 3: Residential Living Facilities
When home care is no longer sufficient, residential facilities offer more comprehensive support. The table below compares the main options.

| Feature | Assisted Living | Memory Care | Nursing Homes |
|---|---|---|---|
| Level of Care | Support with ADLs, medication management | Specialized, 24/7 care for memory impairment | 24/7 skilled nursing care, medical supervision |
| Staffing | 24/7 staff for assistance | Specially trained staff in dementia behavior management | Registered nurses, aides, therapists |
| Environment | Residential, homelike, less restrictive | Secure, thoughtfully designed to prevent wandering | Clinical, hospital-like setting |
| Resident Profile | Needs help with ADLs but mostly independent | Moderate to severe memory loss, behavioral challenges | Complex medical needs, chronic conditions, rehabilitation |
| Activities | Social, recreational, focus on independence | Cognition-stimulating, therapeutic, structured | Therapeutic, often more limited due to medical needs |
Assisted living facilities are for those who need help with daily activities but not constant medical oversight. Memory care communities, like Memory Lane, are specialized environments designed for dementia, with secure layouts, specially trained staff, and therapeutic activities. Nursing homes provide the highest level of medical care for individuals with complex health needs requiring 24/7 skilled nursing.
When Is It Time to Consider a Move to Long-Term Care?
The decision to move a loved one is difficult. Key signs that it may be time include:
- Caregiver burnout: Constant stress, declining health, or emotional exhaustion in the primary caregiver.
- Safety concerns: Repeated falls, wandering, or unsafe behaviors (e.g., leaving the stove on) that cannot be managed at home.
- Escalating medical needs: Conditions requiring skilled nursing care beyond what home health can provide.
- Need for 24-hour supervision: When a person can no longer be left alone safely, which is often financially unsustainable with in-home care.
- Social isolation: A lack of meaningful engagement and companionship at home.
A professional evaluation from a geriatrician or care manager can provide an objective assessment to help guide this decision.
Option 4: Specialized and End-of-Life Care
- Respite care: Provides short-term relief for caregivers, for a few days or weeks. It’s an essential tool for preventing burnout.
- Palliative care: Can begin at any stage of dementia to manage symptoms, improve comfort, and improve quality of life alongside other treatments.
- Hospice care: Focuses entirely on comfort and dignity in the final stages of life, typically when life expectancy is six months or less. Support can be provided at home or in a facility.
For more resources, explore information on getting help with Alzheimer’s caregiving.
Navigating the Search: How to Find, Vet, and Fund Care
Once you know what kind of care is needed, the next step is finding, screening, and funding it. This process requires research and asking tough questions, but resources are available to help.

Finding and Screening Reputable Dementia Care Options
Start your search for dementia care options with trusted sources. Your loved one’s doctor, local Area Agency on Aging, and the Alzheimer’s Association are excellent starting points. Once you have a list of potential providers or facilities, the vetting process begins.
- Visit in person: Go at different times of day to observe staff-resident interactions and the overall atmosphere. Trust your gut.
- Ask about staff training: Inquire specifically about dementia care training and certifications. Staff expertise is critical.
- Check references: Speak with other families who have used the service or facility.
- Review care planning: Ask how care plans are created, updated, and communicated to the family.
Understanding Costs and Financial Assistance
Dementia care can be expensive, but several funding sources may be available.
- Private Pay: Using personal savings, pensions, or other assets.
- Long-Term Care Insurance: If a policy was purchased previously, review it carefully to understand coverage and benefits.
- Medicare: Generally covers short-term skilled care after a hospitalization but does not cover long-term custodial care.
- Medicaid: A federal-state program for low-income individuals that can cover long-term care, but eligibility is strict.
- Veterans (VA) Benefits: The Aid and Attendance benefit can help eligible veterans and spouses pay for care.
Services like the National Council on Aging’s BenefitsCheckUp can help you find programs you may qualify for.
Legal and Financial Planning for the Future
Advance planning is protective, not pessimistic. It ensures your loved one’s wishes are honored and prevents legal crises.
- Power of Attorney (POA): Designates a trusted person to make financial and legal decisions. This must be established while your loved one still has the capacity to do so.
- Healthcare Directives (Living Will): Outlines preferences for medical treatment and end-of-life care.
Consulting an elder law attorney is highly recommended. They specialize in these matters and can help with asset protection, estate planning, and navigating Medicaid rules, potentially saving you from costly mistakes.
Supporting the Supporters: Essential Resources for Caregivers
Behind every person with dementia is often a dedicated caregiver. If that’s you, your well-being is just as important as your loved one’s. Building a support network is not a luxury; it’s essential for the long-term journey of caregiving.

The Importance of Caregiver Self-Care
You cannot pour from an empty cup. Prioritizing your own needs is necessary to provide effective care.
- Take breaks: Use respite care services to give yourself time to rest and recharge. Even short breaks can make a difference.
- Maintain hobbies and social connections: Stay connected to the activities and people that bring you joy and define you outside of your caregiving role.
- Protect your physical health: Prioritize healthy eating and regular exercise. A simple walk can reduce stress and improve your well-being.
- Address your mental health: Acknowledge feelings of stress, guilt, and loneliness. Join a caregiver support group, practice mindfulness, or seek professional help from a therapist. These are signs of strength, not weakness.
Explore more tips on taking care of yourself as a caregiver to build a sustainable routine.
Managing Communication and Behavioral Changes
Changes in communication and behavior are symptoms of the disease, not personal attacks. Responding with patience and compassion is key.
When faced with agitation or aggression, try to identify the underlying cause, such as pain, fear, or an unmet need. Avoid arguing or trying to use logic. Instead, respond to the emotion behind the behavior. Sundowning, or increased agitation in the late afternoon, can be managed with a calm environment, limited caffeine, and a consistent routine.
Two helpful approaches include:
- The 4Rs Approach:Reassure your loved one, Reconsider the cause of distress, Redirect their attention to something pleasant, and help them Relax.
- Validation Therapy: Instead of correcting them, validate their feelings. If they ask for a deceased spouse, say, “You must miss them very much. Tell me about them.” This preserves dignity and reduces anxiety.
For more detailed guidance, review these strategies for managing changes in behavior.
Frequently Asked Questions about Dementia Care
What is the difference between dementia and Alzheimer’s disease?
Think of dementia as an umbrella term for a set of symptoms—including memory loss, and impaired thinking and language—that interfere with daily life. It’s not a specific disease.
Alzheimer’s disease is the most common disease that causes dementia, accounting for 60-80% of cases. It’s a progressive brain disorder caused by the buildup of abnormal proteins. Other causes of dementia include Vascular dementia, Lewy Body dementia, and Frontotemporal dementia. An accurate diagnosis is crucial because different types of dementia require different management approaches.
How can I make the home safer for someone with dementia?
Simple modifications can significantly improve home safety and reduce accidents.
- Remove tripping hazards: Clear clutter, secure rugs, and hide electrical cords.
- Install grab bars: Place them in bathrooms near the toilet and in the shower for stability.
- Secure medications: Lock away all medications to prevent accidental overdose or misuse.
- Use safety locks: Secure cabinets with cleaning supplies and consider locks for stove controls.
- Improve lighting: Use bright, even lighting and night-lights to reduce confusion and prevent falls.
- Prevent wandering: Use door alarms or special locks. Consider a service like the Alzheimer Society’s Finding Your Way® program.
What is the single most important first step when exploring dementia care options?
Getting a thorough medical assessment for an accurate diagnosis is the most critical first step. This foundation is essential because it:
- Guides all care decisions: The specific type and stage of dementia determine the right level of support, activities, and potential treatments.
- Rules out other conditions: Some treatable issues, like vitamin deficiencies or medication side effects, can mimic dementia symptoms.
- Enables proactive planning: A clear diagnosis allows for honest family conversations about care preferences, finances, and legal matters while your loved one can still participate.
With a diagnosis, you can effectively consult with professionals like geriatric care managers to find the right dementia care options for your loved one’s specific needs.
Conclusion: Finding a Path Forward with Confidence
Navigating dementia care options can feel overwhelming, but you don’t have to do it alone. The right path is the one that fits your family’s unique needs, and it begins with an honest assessment of where your loved one is today.
This journey involves understanding the full spectrum of care, from in-home support to specialized residential communities. Planning ahead—by getting a medical assessment, exploring financial resources, and having open conversations—gives you the gift of thoughtful preparation, allowing you to adapt as needs change without being in a state of crisis.
At Memory Lane, we’ve walked alongside countless families on this path. We provide 24/7 personalized, compassionate support for individuals with dementia and Alzheimer’s in Ann Arbor, Ypsilanti, Saline, and the Detroit area. Our approach is to create a secure, engaging environment where residents can thrive with dignity. We develop custom care plans that evolve with each resident, focusing on enhancing quality of life and preserving independence.
Educating yourself is a loving and powerful first step. Whether your loved one remains at home or transitions to a community like ours, what matters most is that they receive compassionate care that honors who they are.
Learn more about specialized memory care in Detroit, Michigan and find how Memory Lane can support your family’s journey.



