Explore assisted living mi options: costs, regulations, and finding the right care in Michigan for your loved one. Get peace of mind.

Dementia Care Planning: Your Step-by-Step Guide for Nursing Home Residents
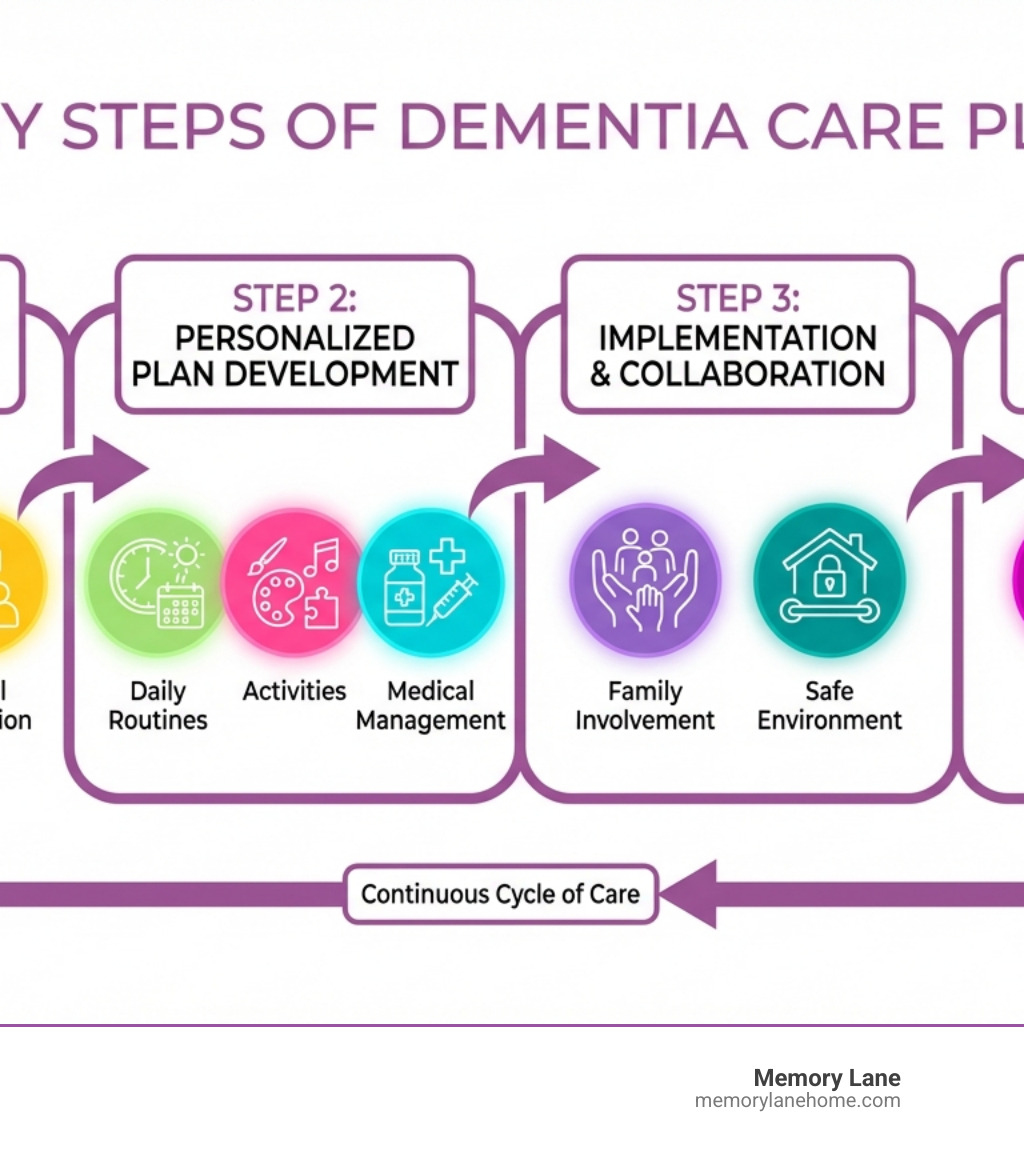
Care plan for dementia patient in nursing home: 4-Step Blueprint
Why a Care Plan for Dementia Patient in Nursing Home Is Essential
A care plan for dementia patient in nursing home is a personalized guide outlining strategies to support an individual’s cognitive, physical, emotional, and social needs. A comprehensive plan includes:
Core Components of a Dementia Care Plan:
- Assessment: A thorough evaluation of cognitive status, medical history, daily living abilities, and personal preferences.
- Personalized Goals: Measurable objectives focused on maintaining dignity, independence, and quality of life.
- Daily Care Strategies: Detailed routines for meals, medication, personal care, activities, and behavioral support.
- Safety Measures: Environmental modifications and interventions to prevent falls, wandering, and other risks.
- Regular Updates: Scheduled reviews and adjustments as dementia progresses.
This roadmap is critical because more than 50 percent of nursing home residents have some form of cognitive impairment. Without a structured plan, care is reactive, not proactive, and residents miss opportunities for comfort and connection. Research shows that structured activities can reduce agitation and improve mood. A well-designed care plan honors the whole person, their life story, and what brings them joy.
I’m Jason Setsuda, a Board Certified Emergency Medicine Physician and CFO of Memory Lane Assisted Living. I’ve spent years developing effective care plans for dementia patients in nursing homes that prioritize medical excellence and person-centered support. My experience in emergency medicine, hospice, and long-term care administration provides a comprehensive understanding of what works for residents with cognitive decline.
Learn more about care plan for dementia patient in nursing home:
- does medicare cover nursing home care for dementia patients
- memory loss assisted living
- assisted living facility near me
Step 1: The Foundation – Comprehensive Resident Assessment

An effective care plan for dementia patient in nursing home begins with understanding the person behind the diagnosis. This person-centered approach involves gathering information on their health, history, and habits to create a holistic view that captures the whole person, not just their symptoms.
Assessing Cognitive, Physical, and Psychosocial Needs
Our assessment looks at multiple dimensions of a resident’s life. We evaluate cognitive status (memory, attention, language) using tools like the MMSE or MoCA to guide communication and support. We also assess physical health, including mobility, balance, and strength, to encourage independence while ensuring safety. Since dementia increases fall risk due to its effects on judgment and coordination, we conduct detailed fall risk assessments.
We evaluate Activities of Daily Living (ADLs)—such as bathing, dressing, and eating—to provide the right amount of support without undermining dignity. Sensory function is also checked, as untreated vision or hearing loss can mimic worsening dementia. Addressing these deficits can significantly improve a resident’s engagement.
Gathering a resident’s life history is key. Knowing their hobbies, career, and routines helps us create meaningful activities and understand triggers for distress or comfort. Understanding the emotional journey of dementia patients allows for a deeper connection. Finally, we monitor emotional well-being, as anxiety and depression are common but treatable challenges.
The Role of Diagnostic and Medical Information
A complete care plan requires solid medical information. Knowing the specific type of dementia (e.g., Alzheimer’s, vascular) and its stage of progression helps us anticipate challenges and tailor interventions. Understanding the difference is crucial, as explained in Dementia vs. Alzheimer’s Disease.
We integrate care for co-existing conditions like diabetes or heart disease, as they interact with dementia symptoms. A thorough medication review is also essential to identify drugs that may worsen cognitive symptoms, using resources like the AGS Beers Criteria for Potentially Inappropriate Medication Use.
Lab test results and brain imaging can reveal reversible causes of cognitive changes, such as infections or nutritional deficiencies, and help rule out other conditions. These tools provide a clearer picture for creating the most effective care plan. You can learn more about understanding accurate tests for Alzheimer’s diagnosis. This comprehensive assessment is the living foundation of personalized care.
Step 2: Building a Personalized Care Plan for a Dementia Patient in a Nursing Home

After the assessment, our interdisciplinary team crafts a care plan for dementia patient in nursing home that is as unique as the person it serves. This living document uses individualized goals and custom interventions to anticipate challenges, create joy, and promote independence.
Key Components of a Comprehensive Plan
A comprehensive plan touches every aspect of daily life. Medical management includes medication schedules, side-effect monitoring, and physician coordination. Personal care routines are built around individual preferences, supporting residents’ abilities rather than taking over. Custom activities are designed based on life stories and current abilities, including:
- Music and Art Therapy: To spark creative connection.
- Reminiscence Therapy: Tapping into long-term memories with photos and stories.
- Gentle Exercise: To maintain physical function and improve mood.
- Social Engagement: Group and one-on-one interactions to combat isolation.
- Spiritual Support: Facilitating religious or spiritual practices as desired.
A predictable daily rhythm reduces anxiety. These personalized care plans in Assisted Living Ypsilanti are essential because a one-size-fits-all approach fails in dementia care.
Strategies for Nutrition, Hydration, and Medication
Mealtime support involves creating pleasant social experiences and providing modified diets (pureed or soft foods) for those with swallowing difficulties. We use adaptive utensils and offer small, frequent meals or finger foods as needed. Proper hydration is maintained with accessible hydration stations and preferred beverages to prevent confusion caused by dehydration.
Medication administration requires careful management to reduce polypharmacy, using guidelines like the AGS Beers Criteria for Potentially Inappropriate Medication Use. If a resident resists medication, we use gentle techniques like offering it at a better time or with food, avoiding force.
Managing Behavioral and Psychological Symptoms (BPSD)
We treat behaviors like agitation or wandering as communication of an unmet need. Our approach is to first identify triggers by observing what precedes an episode. We then use non-pharmacological interventions:
- The 4Rs: Reassure with a calm presence, Reconsider the resident’s perspective, Redirect to a pleasant activity, and help them Relax.
- Validation Therapy: Instead of correcting, we validate the underlying emotion to reduce distress.
- Sundowning Strategies: We use structured evening routines, calming activities, and optimized lighting to manage late-day confusion.
- Wandering Management: We provide safe, secure spaces for movement and redirect the impulse with meaningful activities.
Our team is experienced in a wide range of interventions, as detailed in what types of dementia care services are available, and we adapt our methods to best serve each resident.
Step 3: Implementation and Collaboration for Success
A well-designed care plan for dementia patient in nursing home is only effective when implemented with consistent, compassionate teamwork. Collaboration between staff, families, and the resident transforms a written plan into daily moments of dignity and connection.
The Crucial Role of Family Involvement in the care plan for a dementia patient in a nursing home
Families are the experts on their loved ones, and their insights are the building blocks of person-centered care. We partner with families through:
- Collaborative Goal-Setting: We work together to define what success looks like, whether it’s maintaining mobility or finding moments of joy.
- Sharing Personal Stories: Knowing a resident’s history helps our team connect with them as an individual and tailor activities that honor their identity.
- Regular Care Conferences: We hold meetings to review progress, hear concerns, and make adjustments together, maintaining open communication between visits.
- Support Resources: We connect families with community resources like support groups and educational programs. Choosing the best dementia care homes for reliable support often means finding a facility that values this partnership.
Creating a Safe and Supportive Environment
Our environment is designed to be both safe and homelike. Fall prevention is a top priority, with clear, well-lit pathways, grab bars, and activities that maintain strength. Our secure spaces in Ann Arbor, Ypsilanti, and Saline allow for safe exploration, preventing wandering into unsafe areas. You can learn more about our approach at our dementia care facilities Grosse Ile Township Michigan location.
Clear signage with pictures and simple words helps residents steer independently, preserving dignity. We also create a homelike atmosphere while reducing confusing stimuli like loud noises or visual clutter, which can trigger agitation.
Navigating Legal and Ethical Considerations
Protecting a resident’s rights and wishes is essential. We uphold every resident’s right to dignity, privacy, and respect. Key legal and ethical considerations include:
- Advance Directives: Documents like a living will outline medical treatment preferences. We help ensure these are in place and followed.
- Power of Attorney: This designates a trusted person to make healthcare or financial decisions when the resident cannot.
- Informed Consent: We involve residents in decisions as long as they have capacity. As capacity diminishes, we work with their designated representative.
- Decision-Making Capacity: We continually assess capacity, as it can fluctuate, respecting a resident’s remaining abilities while ensuring their well-being.
The National Institute on Aging provides helpful guidance on advance care planning health topic from NIA.
Step 4: Adapting the Plan as Needs Evolve
Dementia is progressive, so an effective care plan for dementia patient in nursing home must be a living document that adapts to a resident’s changing needs. As Alzheimer’s progresses, abilities change, and what works one month may need adjustment the next. This flexibility is the core of responsive, high-quality care.
Regular Review and Updates to the care plan for a dementia patient in a nursing home
Keeping a care plan current requires continuous communication and vigilance. Our key practices include:
- Scheduled Reviews: We conduct formal reviews at least quarterly with the resident, family, and our interdisciplinary team to discuss what’s working and what needs to change.
- Immediate Re-assessment: We don’t wait for a scheduled review. Any significant shift in a resident’s cognitive, physical, or behavioral condition triggers an immediate re-assessment to understand the “why” behind the change.
- Careful Documentation: Every adjustment is documented to track patterns, inform future decisions, and ensure continuity of care among all team members.
- Clear Communication: All changes to the care plan are clearly communicated to the entire care team and family members to ensure care is coordinated and effective.
This commitment to continuous improvement is crucial. Families exploring options should discover what to look for in local memory care facilities that prioritize this kind of adaptive planning. We see each adjustment as an opportunity to better serve our residents and maximize their quality of life at every stage.
Frequently Asked Questions about Dementia Care Plans
Here are answers to common questions about care plans for dementia patients in nursing homes.
How often should a dementia care plan be reviewed?
A care plan for dementia patient in nursing home is a living document. We formally review each plan at least every three months and anytime there is a significant change in a resident’s condition. A significant change could be a shift in cognitive abilities, a new behavior, a fall, or a change in health status. Regular reviews ensure the plan remains effective and serves the resident’s current needs.
Can a family member disagree with the care plan?
Yes, absolutely. Family input is vital. If you disagree with any part of the plan, we see it as an opportunity for a productive conversation. We will schedule a care conference with our interdisciplinary team to discuss your concerns and work collaboratively to find a solution. Your insights into your loved one’s history and preferences are irreplaceable for creating the best care plan.
What is “person-centered care” in a dementia care plan?
Person-centered care means prioritizing the individual over the diagnosis. Instead of just managing symptoms, we focus on the person’s life story, values, and preferences. When creating a care plan for dementia patient in nursing home, we ask: Who is this person? What brings them joy and comfort? This information guides everything from daily routines to activities. For example, we might play a resident’s favorite music or schedule activities based on their lifelong habits. This approach respects dignity, honors individuality, and transforms care from a set of tasks into a compassionate relationship.
Conclusion: A Path to Improved Quality of Life
An effective care plan for dementia patient in nursing home is a living commitment, not a static document. The four steps—assessment, personalized planning, collaborative implementation, and continuous adaptation—create a roadmap that honors the whole person. This proactive approach leads to remarkable outcomes: reduced anxiety, increased connection, and a sense of purpose for residents.
A well-crafted plan preserves dignity, maintains safety, and ensures every resident is valued for who they are. At Memory Lane, our philosophy is built on this compassionate process. In Ann Arbor, Ypsilanti, Saline, and across Michigan, we are committed to creating personalized care plans that make a real difference.
If you are seeking specialized dementia care that goes beyond the basics, we invite you to learn how our individualized plans improve quality of life. Discover our memory care services to see how we can help.


