Unlock expert steps for a compassionate care plan for dementia patient in nursing home. Enhance quality of life & dignity today.

Beyond the Bill: A Deep Dive into Alzheimer’s Financial Burden
Cost of Alzheimer’s: Staggering $360B Burden in 2024
The Growing Financial Crisis of Alzheimer’s Disease
The cost of Alzheimer’s is staggering and growing rapidly. Here’s what you need to know:
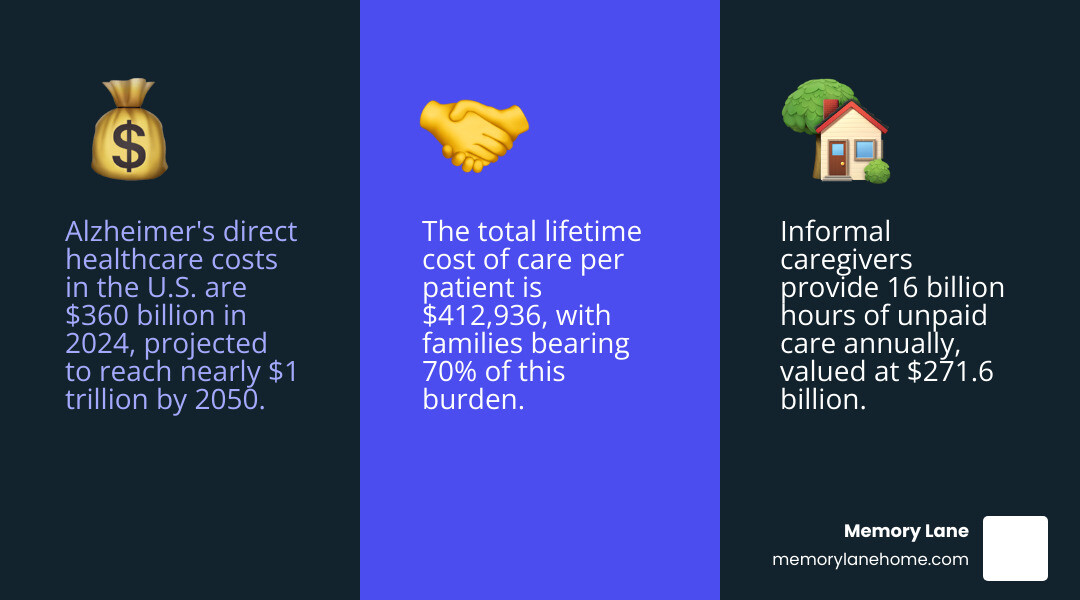
- Total U.S. cost in 2024: $360 billion in direct healthcare expenses
- Projected by 2050: Nearly $1 trillion annually
- Medicare and Medicaid: Cover 64% of costs ($231 billion)
- Family out-of-pocket: $52-97 billion per year
- Unpaid caregiving value: $271.6 billion (16 billion hours)
- Lifetime cost per patient: $412,936 (70% paid by families)
More than 7 million Americans are living with Alzheimer’s disease today. That number is expected to reach nearly 13 million by 2050. Behind these statistics lies a profound financial reality that touches millions of families every year.
The financial burden of Alzheimer’s extends far beyond hospital bills and medications. It encompasses years of specialized care, countless hours of family caregiving, lost wages, and the emotional toll that comes with watching a loved one’s cognitive decline. For every dollar spent on direct medical care, families bear additional costs through unpaid caregiving time and out-of-pocket expenses.
Medicare and Medicaid shoulder the majority of direct healthcare costs, spending an average of 3 times more per person with dementia than for seniors without the disease. Yet this represents only part of the story. Family caregivers provide nearly 16 billion hours of unpaid care annually—time that carries both an economic value and a personal cost measured in missed work, depleted savings, and diminished health.
The numbers are sobering, but understanding them is crucial for families beginning this journey. Early planning and access to specialized support can make a significant difference in both financial outcomes and quality of life.
I’m Jason Setsuda, a Board Certified Emergency Medicine Physician and CFO of Memory Lane Assisted Living with over 15 years of business management experience. Through my work with families navigating the cost of Alzheimer’s care, I’ve seen how proper planning and specialized support can ease both the financial and emotional burden of this disease.
The Staggering Price Tag: Unpacking the Direct Cost of Alzheimer’s
When we talk about the cost of Alzheimer’s, we often begin with the most tangible expenses: the medical bills, the long-term care facility fees, and the prescription drugs. These are the direct costs, and they represent a monumental financial challenge for individuals, families, and the entire healthcare system.
The National Cost of Alzheimer’s: Current and Projected Figures
The current estimated total healthcare cost of Alzheimer’s disease and related dementias in the United States is staggering. In 2024, the direct costs to American society for caring for those with Alzheimer’s and other dementias will total an estimated $360 billion. This figure encompasses all the medical and long-term care expenses associated with managing this progressive disease.
But the financial burden isn’t static; it’s a rapidly escalating crisis. These costs are projected to change dramatically in the coming years. As the population ages, the number of individuals living with Alzheimer’s is expected to surge. The number of Americans aged 65 and older is projected to grow from 58 million in 2022 to 82 million by 2050. Consequently, the number of Americans living with Alzheimer’s will nearly double by 2050 to 12.7 million if nothing changes. This demographic shift means that the total cost of treating individuals with Alzheimer’s is projected to exceed $1 trillion annually by 2050.
To put this into perspective, Alzheimer’s is currently one of the most expensive diseases in America, costing more than cancer and heart disease combined. In the last five years of life, the costs for a person with dementia average more than $287,000 (in 2010 dollars), compared with $175,000 for heart disease and $173,000 for cancer. This comparison underscores the immense scale of the financial challenge posed by Alzheimer’s.
Breaking Down Healthcare Expenses
So, what are the primary components that make up this colossal sum? The direct costs of care for Alzheimer’s disease are primarily attributed to:
- Skilled Nursing Care: As the disease progresses, many individuals with Alzheimer’s require 24/7 supervision and specialized medical care that can only be provided in a skilled nursing facility. These facilities offer comprehensive medical, personal, and rehabilitative care.
- Home Healthcare: For those who can remain at home, professional home healthcare services provide assistance with daily activities, medication management, and skilled nursing tasks. This allows individuals to age in place longer, but it still represents a significant expense.
- Hospice Care: In the advanced stages of Alzheimer’s, hospice care focuses on comfort and quality of life, providing medical, emotional, and spiritual support to patients and their families.
- Hospital Stays and Doctor Visits: Individuals with Alzheimer’s often experience higher rates of hospitalizations and require frequent doctor visits to manage symptoms, comorbidities, and complications.
- Prescription Drugs: While disease-modifying treatments are still emerging, managing symptoms and co-occurring conditions often requires a range of prescription medications.
Our research shows that the average total annual costs in 2021 dollars for Medicare beneficiaries 65 years and older with Alzheimer’s disease or other dementias have been estimated to be $41,757. This is about three times higher than the $14,026 spent on those without Alzheimer’s. This disparity highlights the intensive and prolonged care needs associated with the disease.
The Role of Medicare and Medicaid
When we examine who bears the brunt of these direct costs, government programs like Medicare and Medicaid emerge as major payers. In 2024, Medicare and Medicaid will spend an estimated $231 billion caring for those with Alzheimer’s and other dementias, accounting for a substantial 64% of the total direct costs.
Medicare, designed primarily for seniors, faces a significant burden. Average per-person Medicare spending for seniors with Alzheimer’s is 2.8 times higher than average per-person spending for all other seniors. This means that nearly one in every six Medicare dollars will be spent on someone with Alzheimer’s in 2024.
Medicaid, which provides healthcare for low-income individuals and long-term care for many, also sees a disproportionate impact. Under Medicaid, spending on individuals with Alzheimer’s is, on average, more than 22 times higher than for seniors without the disease. For instance, the average annual Medicaid costs for Medicare beneficiaries with Alzheimer’s were $6,478, compared to just $291 for those without. These figures underscore the critical role these programs play in supporting Alzheimer’s care, but also the immense financial pressure they face. You can explore more about the economic and societal burden of Alzheimer’s disease from a managed care perspective here.
The Hidden Toll: Indirect Costs and the Burden on Families
While direct medical and long-term care costs are substantial, they represent only one part of the financial equation. The true cost of Alzheimer’s is far greater when we consider the indirect costs – the often-unseen financial and personal sacrifices made by families and caregivers. These hidden tolls constitute a massive portion of the disease’s true economic and societal burden.
The Immense Value of Informal Caregiving

Perhaps the most significant indirect cost comes from informal caregiving. Across the United States, millions of family members and friends step into the role of caregiver, providing round-the-clock support without financial compensation. Our research indicates that nearly 12 million family and unpaid caregivers provided an estimated 19 billion hours of informal assistance in 2024. The economic value of this unpaid care is truly staggering, estimated at approximately $413.4 billion annually.
This immense contribution from informal caregivers is often overlooked in traditional cost analyses, yet it is absolutely crucial to the well-being of individuals with Alzheimer’s. These are husbands, wives, children, siblings, and friends who provide everything from personal care and meal preparation to transportation and emotional support. Without their dedication, the direct healthcare system would be utterly overwhelmed. The societal contribution of these caregivers cannot be overstated; they are the backbone of Alzheimer’s care.
Out-of-Pocket Expenses: The Family’s Financial Strain
Beyond the unpaid labor, families also face substantial out-of-pocket expenses. The total lifetime cost of care for a patient with dementia is estimated at $412,936 (in 2022 dollars). Crucially, a staggering 70% of these costs are borne by family caregivers, either through direct out-of-pocket health and long-term care expenses or from the economic value of their unpaid care.
For caregivers, these direct financial burdens are significant. Dementia caregivers bore nearly twice the average out-of-pocket costs of non-dementia caregivers, spending an average of $12,388 annually compared to $6,667. In 2024, out-of-pocket spending by patients, their families, and their caregivers is projected to be $97 billion. The average yearly out-of-pocket expense per person for Medicare beneficiaries aged 65 and older with dementia is $10,289. These figures highlight the severe financial strain placed directly on families, often depleting savings and impacting their financial security for years to come.
The Caregiver’s Sacrifice: Lost Wages and Health
The impact of caregiving extends further, significantly affecting caregivers’ own financial well-being and productivity. The demanding nature of Alzheimer’s care often forces caregivers to make difficult choices about their careers:
- Lost Earnings: Lost earnings among friends and family who forego work or reduce their hours to provide care total an estimated $8.2 billion annually.
- Reduced Work Hours and Early Retirement: A significant percentage of caregivers – 56% in 2023 – reported retiring early, cutting back their work hours, or even resigning from or losing their jobs specifically to provide care for someone with Alzheimer’s disease. This loss of income can have long-lasting effects on a family’s financial stability and future retirement plans.
Moreover, the physical and mental toll on caregivers is immense, leading to their own increased healthcare costs and diminished quality of life. Household members caring for patients with Alzheimer’s have significantly higher average annual healthcare costs ($7,168) compared to those not caring for someone with Alzheimer’s ($6,301). Nearly three-fourths of dementia caregivers report concern about maintaining their own health, and approximately 40% suffer from depression and anxiety. This highlights how the disease doesn’t just affect the patient; it profoundly impacts the health and well-being of their entire support system. The decline in quality of life for care partners alone is valued at $6 billion.
Navigating the Financial Landscape and Planning for the Future
The numbers surrounding the cost of Alzheimer’s can feel overwhelming, painting a daunting picture for families in Michigan and across the country. However, understanding these costs is the first step toward proactive planning. By focusing on early action, understanding available care options, and leveraging support systems, we can help steer this challenging financial journey.
Managing the Future Cost of Alzheimer’s with Early Diagnosis
Early diagnosis and treatment of Alzheimer’s disease hold significant potential for better outcomes and, importantly, lower overall costs in the long run. When an individual receives a timely diagnosis, it opens doors to:
- Cost-Saving Potential: Studies indicate that patients who consulted a specialist upon initial indication of cognitive decline led to a timelier diagnosis of Alzheimer’s and significantly lower all-cause medical costs in the first year after diagnosis. This is because early diagnosis allows for better management of symptoms and comorbidities, potentially delaying the need for more expensive, intensive care later.
- Timely Financial Planning: An early diagnosis provides families with crucial time to understand the disease progression, explore financial resources, and make informed decisions about long-term care planning. This proactive approach can help mitigate future financial shocks.
- Access to Support Resources: Early diagnosis connects families with support groups, educational programs, and professional services that can help them cope with the challenges of the disease, manage symptoms, and plan for the future.
We encourage open conversations with healthcare providers about any concerns regarding cognitive changes. For families in Ann Arbor, Ypsilanti, or Saline, Michigan, seeking a specialist early on can make a profound difference.
The Evolving Landscape of Alzheimer’s Care
The field of Alzheimer’s care is constantly evolving, with advancements in understanding the disease and developing new treatments. These changes will undoubtedly influence future healthcare costs. New treatments and blood tests are emerging, and researchers are actively modeling their potential impact on future costs. While the emergence of disease-modifying therapies may help preserve cognitive function, whether they will reduce overall healthcare costs remains to be seen, as new therapies often come with high price tags.
Amidst these developments, the importance of specialized memory care continues to grow. Facilities like ours, Memory Lane, focus on improving symptoms of Alzheimer’s and related dementias to improve patient outcomes, quality of life, and reduce healthcare costs by providing custom, comprehensive support. Our goal is to create supportive environments that allow individuals to maintain dignity and independence for as long as possible.
Managed care organizations also play a crucial role in reducing the economic burden of Alzheimer’s. They are uniquely positioned to develop utilization strategies that positively impact early diagnosis and treatment, leading to better outcomes and lower costs for patients, caregivers, and the healthcare system. The inclusion of Alzheimer’s disease diagnoses into risk corridor calculations by CMS may even encourage Medicare Advantage organizations to invest more in early detection and diagnosis programs.
Memory Care Options and Their Associated Costs
Understanding the different care options and their associated costs is vital for families planning for the future. In Michigan, as elsewhere, options range from in-home care to specialized memory care communities.
Here’s a comparison of average monthly costs and services in Michigan:
| Care Option | Average Monthly Cost (Michigan) | Key Services |
|---|---|---|
| Home Care | $3,360 – $5,760 (National Average) | Personal care assistance (bathing, dressing), companionship, light housekeeping, meal preparation, medication reminders (non-medical). Allows individuals to remain in their own homes. Costs can vary significantly based on the number of hours per week and the level of care required. |
| Memory Care Community | ~$5,213 (Michigan Median, up to $10,435) | 24/7 supervision by specially trained staff, personalized care plans, memory-stimulating activities (art, music therapy), secure environment designed to minimize confusion and wandering, nutritious meals, medication management, emotional support, and social engagement. Provides a structured and safe environment with specialized programming for cognitive impairment. |
Note: These are average costs and can vary widely based on location within Michigan (e.g., Ann Arbor, Ypsilanti, Saline), the specific facility, apartment size, amenities, and the individual’s level of care needs.
Memory care communities, while often perceived as more expensive, offer specialized support that extends beyond basic personal care. They provide a secure environment, structured activities custom to cognitive abilities, and staff trained specifically in dementia care. For many families, this comprehensive approach offers peace of mind and can alleviate the immense burden on informal caregivers.
For more detailed information on dementia care services and how we can help, please visit our dedicated page on dementia care services.
Frequently Asked Questions about Alzheimer’s Costs
How much does Alzheimer’s care cost the United States annually?
The total direct cost for caring for Americans with Alzheimer’s and other dementias is estimated to be $360 billion in 2024. This does not include the hundreds of billions of dollars in unpaid care provided by family members.
Who pays for most of the direct costs of Alzheimer’s care?
Government programs bear the largest share, with Medicare and Medicaid covering approximately 64%, or $231 billion, of the total direct costs in 2024. The remaining expenses are paid out-of-pocket by individuals and their families.
What is the estimated total lifetime cost of care for a person with dementia?
The total lifetime cost of care for an individual with dementia is estimated at $412,936. Crucially, about 70% of this cost is borne by the family through out-of-pocket spending and the value of unpaid caregiving.
Conclusion: Finding Support and Quality Care on the Alzheimer’s Journey
The financial journey of Alzheimer’s is complex and profound, extending far beyond medical bills to impact every facet of a family’s life. Understanding both the direct and hidden costs is the first step toward effective planning and reducing the burden. While the numbers are daunting, proactive planning and finding the right support system can make a significant difference. For families seeking a secure, compassionate, and specialized environment, facilities like Memory Lane provide custom programs that focus on enhancing quality of life for residents. By choosing dedicated memory care, families can ensure their loved ones receive the expert attention they need, providing peace of mind. Learn more about professional dementia care.



