Unlock expert steps for a compassionate care plan for dementia patient in nursing home. Enhance quality of life & dignity today.

Finding the Perfect Fit: A Comprehensive Look at Dementia Housing and 24/7 Care
Long-Term Dementia Care: Your 24/7 Perfect Fit
Understanding the Path to Long-Term Dementia Care
Long-term dementia care provides specialized residential support for individuals with dementia who need 24-hour supervision, personalized assistance, and a secure environment. Here’s a brief overview:
Key Long-Term Care Options:
- Memory Care Communities: Secure, specialized facilities with trained staff and dementia-specific programming.
- Assisted Living with Memory Support: A less intensive option for early-stage dementia.
- Skilled Nursing Homes: For those with complex medical needs alongside dementia.
- Continuing Care Retirement Communities (CCRCs): Offer multiple care levels on one campus.
When to Consider Long-Term Care:
- Safety concerns at home (wandering, falls).
- Caregiver stress or burnout.
- A need for 24-hour supervision.
- Behavioral changes requiring specialized management.
- Medical needs that exceed home care capacity.
Learning a loved one has dementia brings difficult questions: When is it time for residential care? What does quality care look like? These questions are normal, and the decision can feel overwhelming. About one-third of seniors younger than 80 with dementia live in long-term care homes, increasing to 42% for those 80 and older. The goal is to find the right place that honors your loved one’s dignity.
Today’s specialized memory care communities offer person-centered approaches that maintain independence as cognitive abilities change. They feature trained staff, secure environments for safe movement, and activities that promote engagement.
This guide will walk you through recognizing when home care is no longer enough, understanding your options, choosing a community, and navigating costs.
As Jason Setsuda, a Board Certified Emergency Medicine Physician and CFO of Memory Lane Assisted Living, I’ve spent over a decade helping families steer these decisions. My experience has shown me how the right care environment can transform quality of life for both residents and their families.
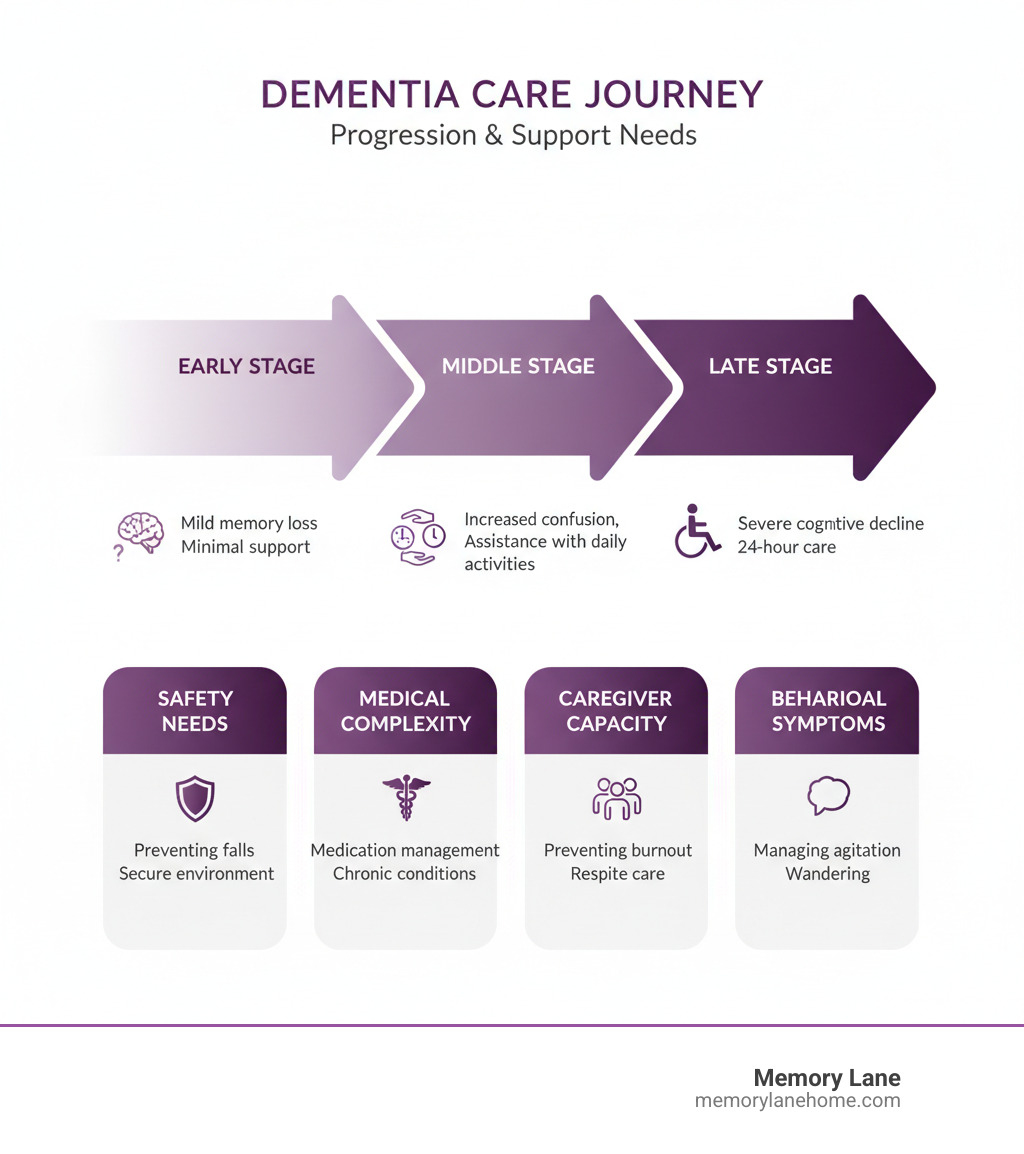
Recognizing When It’s Time for a Change
There’s rarely a single moment when you know it’s time for a change. It’s usually a gradual realization built from close calls, sleepless nights, and the feeling that you can’t keep going. Deciding to move a loved one into long-term dementia care is one of life’s hardest decisions, often mixing guilt and sadness with relief. It’s not giving up; it’s recognizing that love sometimes means finding help beyond what you can provide alone.
Caregiver burnout is more than just fatigue. It’s emotional and physical exhaustion that affects your health, relationships, and well-being. When you find yourself neglecting your own needs or your doctor is concerned about your health, the situation is no longer sustainable.
Safety concerns often force the conversation. Wandering is a terrifying risk, and the risk of falls is significantly higher for those with dementia. Kitchen hazards, like a stove left on, or medication errors also signal that home may no longer be the safest place. Behavioral changes like sundowning (late-day confusion and agitation) or aggression can be heartbreaking and difficult to manage without specialized, 24-hour support. Finally, social isolation can affect both the person with dementia and the caregiver, making a community setting a more engaging and supportive choice.
Key Signs Your Loved One May Need More Support
Watch for these practical signs that home care may no longer be enough. A consistent struggle with Activities of Daily Living (ADLs)—bathing, dressing, eating, and mobility—is a clear indicator. Difficulties with more complex Instrumental Activities of Daily Living (IADLs), such as meal preparation or managing finances, are also important. Medication management errors are particularly dangerous. A noticeable decline in personal hygiene or an unsafe home environment (clutter, spoiled food) are also red flags. When increased confusion leads to dangerous situations or an inability to recognize family, it’s time to consider more support. The bottom line is when your loved one’s care needs exceed your ability to provide safe, consistent support, exploring long-term dementia care is the right next step.
Evaluating Your Role as a Caregiver
Your role doesn’t end with professional care; it changes. Many caregivers find they can be more present emotionally once the physical demands are lifted. But first, be honest about your own well-being. Caregiver stress can manifest as irritability, frequent illness, or social withdrawal. The emotional toll is immense, often involving guilt over considering residential care and relief at the prospect. This is normal. The physical demands of lifting, transferring, and providing round-the-clock supervision can be overwhelming.
Balancing work and family with caregiving can become impossible, straining your career and other relationships. Your own well-being is not selfish—it’s essential. You cannot be an effective advocate for your loved one if you are depleted. Seeking support from family and professionals is a sign of strength. Talk to your loved one’s doctor, connect with other caregivers, and consider support groups. Considering long-term dementia care means ensuring your loved one gets the specialized support they need while you preserve your own health and your relationship with them.
Exploring Your Options for Long-Term Dementia Care

Once you realize home care is no longer enough, the search for the right long-term dementia care setting begins. This is about finding a place where your loved one can be safe, engaged, and cared for by people who understand dementia.
Modern communities focus on person-centered care, treating your loved one as a unique individual. This approach is supported by 24-hour supervision from trained staff who can respond with patience and compassion. These communities also provide secure environments that allow for “sheltered freedom”—safe movement without constant restriction—and engaging activities that bring purpose and joy.
At Memory Lane, we’ve built our entire approach around these principles, creating a place that feels like home, not a hospital.
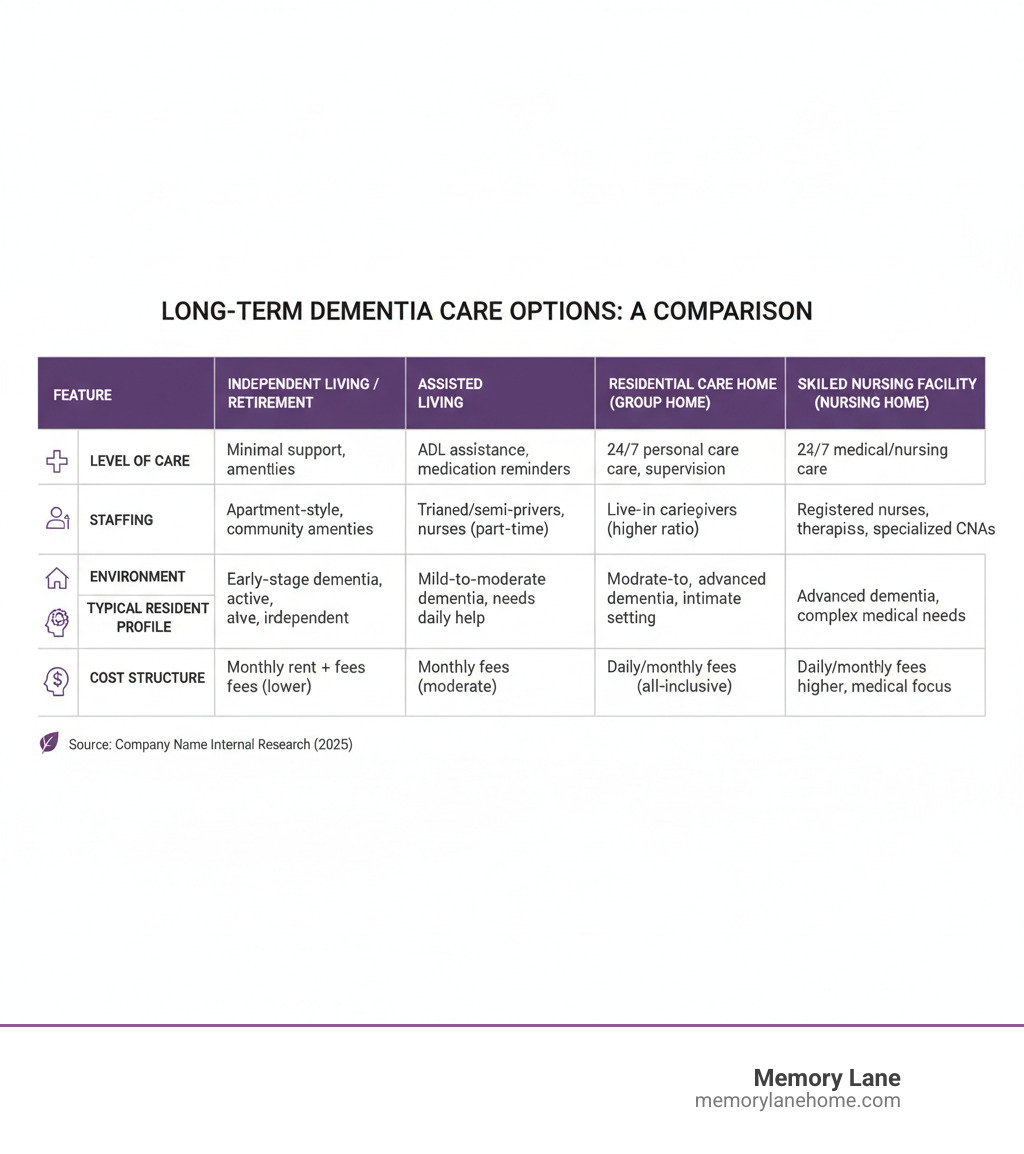
Understanding the Spectrum of Long-Term Dementia Care Settings
Not all residential care is the same. Matching your loved one’s needs to the right setting is key.
- Retirement housing or independent living: Best for early-stage dementia with minimal support needs.
- Assisted living facilities: Offer help with daily tasks, but dementia care specialization varies. You must ask about their specific training and experience.
- Group homes or residential care homes: Provide a smaller, home-like setting for a handful of residents.
- Skilled nursing facilities (nursing homes): Provide 24/7 licensed nursing for complex medical needs alongside dementia care.
- Continuing care retirement communities (CCRCs): Offer multiple levels of care on one campus, allowing residents to transition as needs change.
- Adult day centers: Provide daytime supervision and activities, offering respite for caregivers.
In recent years, 69% of residents in long-term care homes had dementia, showing these communities are designed for people with similar challenges.
What is a Specialized Memory Care Community?
A specialized memory care community adapts the best of assisted living specifically for dementia. They are thoughtfully designed from the ground up.
Purpose-built design is crucial. You’ll find features like circular hallways to prevent confusion, clear pictorial signage, and lighting that reduces shadows. Safe outdoor spaces, like enclosed gardens, allow residents to enjoy fresh air without risk.
Dementia-specific programming focuses on activities that tap into long-term memories and preserved abilities, such as folding laundry, singing familiar songs, or sorting items. These dignified activities maintain a sense of purpose. A higher staff-to-resident ratio allows for more personalized attention and care.
Most importantly, staff are trained in dementia communication and behavior management. They learn to understand that challenging behaviors are often a form of communication. At Memory Lane, our “consistent assignment” approach helps build trust between residents and their regular caregivers. Finally, secured environments provide safety without feeling restrictive, offering sheltered freedom within a protected space.
The Essential Checklist for Choosing a Community

Finding the right long-term dementia care community requires some detective work. You’re searching for a place where your loved one will be treated with dignity and respect.
Start by visiting several communities. Schedule official tours, but also drop by unannounced at different times of day to get a more honest picture of daily life. Observe how staff interact with residents. Is the community clean? Does it feel like a home? Trust your gut—if something feels off, it probably is.
List of Critical Questions to Ask During Your Visit
Use this list to guide your conversations and uncover what really matters for quality care.
- Staffing and Training: Ask about the staff-to-resident ratio (day and night), the specifics of their dementia care training, staff turnover rates, and how they handle challenging behaviors.
- Resident Life and Activities: Request an activity calendar. Ask how they personalize activities and if they offer specialized therapies like music or art.
- Medical Care and Safety: Inquire about medication management, protocols for a fall or medical emergency, and their “aging in place” policy. Will your loved one have to move if their needs increase?
- Environment and Meals: Can residents bring personal items to make their room feel like home? How do they accommodate special diets and assist residents who need help eating?
For a more detailed checklist, the Alzheimer Society offers excellent resources on Long-term care.
Evaluating Quality and Safety
Beyond asking questions, you need to verify the information you receive.
Review the latest inspection reports. For nursing homes, use Medicare’s Nursing Home Compare website. For assisted living, ask the community directly for their state reports. Also, check that the facility is properly licensed by your state and look for certifications from organizations like the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO).
During your visits, use your senses. A well-run community should be clean and free of unpleasant odors. Residents should appear well-groomed and appropriately dressed. Watch staff interactions for patience and respect. If possible, talk to other families to get their honest feedback.
Be aware of quality indicators. While progress has been made in reducing restraint and inappropriate antipsychotic use, residents with dementia still face higher rates of these issues and falls. This highlights the importance of your ongoing advocacy. Resources like The National Long-Term Care Ombudsman Resource Center can provide additional support.
Navigating Costs and Financial Assistance
The cost of long-term dementia care is a significant concern for many families. Understanding your financial options early can reduce stress down the road. The financial landscape can feel complex, but you don’t have to steer it alone.
The Cost of Care: What to Expect
Quality dementia care is a major investment. According to Genworth’s national cost of care data, assisted living facilities average $70,800 per year, while nursing homes can cost over $111,000 annually.
Memory care communities like Memory Lane typically have a higher premium than standard assisted living. This is due to specialized features like higher staff-to-resident ratios, secure environments, and advanced staff training. Costs vary by location; for example, rates in Ann Arbor or Ypsilanti may differ from national averages. When evaluating costs, always ask what’s included in the base rate versus what is charged separately to avoid surprises.
Financial Planning for Long-Term Dementia Care
Most families use a combination of sources to cover care costs. Here are the most common options:
- Private Pay: Using personal savings, retirement income, or investments. This offers the most flexibility.
- Long-Term Care Insurance: If a policy was purchased years ago, it can be a great help. Review the policy carefully for coverage details, waiting periods, and benefit limits.
- Veterans Benefits: Eligible veterans may qualify for various care services. The application can be complex, but veterans’ service organizations can provide free assistance.
- Medicaid: This becomes an option once personal assets are spent down to state-mandated levels. It can cover care in nursing homes and some assisted living facilities. The rules are intricate, so consulting an elder law attorney is highly recommended to steer eligibility and protect assets where possible.
- Medicare: This is often misunderstood. Medicare does not pay for long-term custodial care (the type of care in assisted living or memory care). It may cover short-term skilled nursing care after a qualifying hospital stay, but it is not a long-term solution.
Other options include life insurance conversions, annuities, or reverse mortgages. For more information, visit LongTermCare.gov, a resource from the U.S. Department of Health and Human Services. Planning now provides more options and less stress later.
Ensuring a Smooth Transition and Quality Ongoing Care

Moving a loved one into a long-term dementia care community is the start of a new chapter. Your role evolves from hands-on caregiver to advocate, family connection, and champion for quality care. With thoughtful preparation, this transition can be smoother than you might expect.
Making the Move Easier for Everyone
Creating continuity and comfort is key to a successful move.
- Personalize their new space. Bring familiar items like a favorite chair, photos, or a cherished quilt. These touchstones provide comfort and help staff get to know your loved one.
- Create a memory book for staff. Use a tool like the Alzheimer Society’s “All about me” booklet to share your loved one’s life story, preferences, and routines. This enables truly person-centered care.
- Establish a routine for visits. Consistency helps, but be flexible. Shorter, more frequent visits may be less overwhelming at first. Visiting during an activity can also ease goodbyes.
- Manage your own emotions. It’s normal to feel a mix of guilt, sadness, and relief. Connect with a support group like ALZConnected or talk to other families. Your well-being is crucial for you to be an effective advocate.
- Build relationships with staff. Get to know the care team. Share insights about your loved one. This partnership is built on open communication.
The Hallmarks of High-Quality Dementia Care
Quality care goes beyond physical needs to preserve dignity and foster joy.
Person-centered care plans are the foundation. These are individualized roadmaps based on a resident’s unique history and preferences. High-quality communities also invest in ongoing staff training to manage responsive behaviors and support those with severe cognitive impairment compassionately.
A key indicator of quality is the proactive reduction of physical restraints and inappropriate antipsychotic medications. While progress has been made, vigilance is required. Good communities focus on non-pharmacological interventions first. Family involvement in care planning is also essential. You are a vital member of the care team, and your input ensures care remains person-centered.
Your journey transforms, but it doesn’t end. You become your loved one’s voice and their assurance that they remain loved and valued.
Frequently Asked Questions about Long-Term Dementia Care
You’ve likely got questions running through your mind as you consider this significant decision. That’s completely natural. Over the years, we’ve worked with countless families navigating these same concerns, and we want to address the ones we hear most often.
What is the main difference between general assisted living and a memory care community?
General assisted living is for seniors who need help with daily tasks but are cognitively intact. Memory care is a specialized environment designed specifically for individuals with dementia. The key differences include:
- Specialized Staff: Memory care staff receive in-depth training on dementia communication and behavior management.
- Secure Environment: Communities are secured to prevent unsafe wandering, with features like circular hallways and enclosed outdoor spaces.
- Targeted Programming: Activities are designed to be engaging and successful for individuals with cognitive decline.
- 24/7 Supervision: A higher staff-to-resident ratio ensures constant supervision and personalized attention for the unique challenges of long-term dementia care.
How can I ensure my loved one receives good care after they move in?
Your role as an advocate is crucial. To ensure quality care:
- Stay involved. Visit at different times of day to get a full picture of daily life.
- Build relationships with the care team. Share your loved one’s life story and preferences. Good communication makes for better care.
- Attend care plan meetings. Come prepared with observations and questions to actively participate in their care plan.
- Know your resources. If you have concerns, contact your state’s Long-Term Care Ombudsman. You can find your local office through The National Long-Term Care Ombudsman Resource Center.
- Trust your instincts. If something feels wrong, speak up. A quality community will take your concerns seriously.
Does Medicare pay for long-term dementia care?
This is a common point of confusion. Medicare generally does not cover long-term custodial care, which is the type of non-medical support provided in most assisted living and memory care communities.
Medicare is health insurance that may cover short-term skilled nursing care after a qualifying hospital stay (typically up to 100 days). It is not designed for ongoing residential care. Families typically pay for long-term dementia care using private savings, long-term care insurance, Veterans benefits, or Medicaid (once asset limits are met). Consulting an elder law attorney is wise if you anticipate needing Medicaid. The U.S. Department of Health and Human Services also provides helpful information on payment options.
We understand these financial realities can feel overwhelming. That’s why we encourage families to start financial planning conversations early and explore all available resources. Our team is always available to discuss payment options and connect you with helpful resources in our Ann Arbor, Ypsilanti, and Saline communities.
Conclusion
Finding the right long-term dementia care for someone you love is one of life’s most significant decisions. It’s never easy, and it’s perfectly normal to feel a mix of emotions—uncertainty, guilt, relief, and even hope. But at its heart, this decision comes from a place of deep love and a genuine desire to ensure your loved one’s safety, dignity, and well-being.
We’ve walked alongside countless families in Ann Arbor, Ypsilanti, Saline, and throughout Michigan as they’ve steerd this journey. What we’ve learned is that knowledge truly is power. When you take the time to research your options, ask the tough questions, visit communities, and plan thoughtfully, you can find a place that doesn’t just provide care—it creates a home where your loved one can continue to thrive.
The right memory care community offers more than supervision and assistance. It provides a secure environment where individuals can move freely without fear. It offers engaging activities that honor who they are and who they’ve always been. It delivers compassionate, expert care from staff who truly understand dementia and treat every resident with respect and warmth. Most importantly, it gives families peace of mind, knowing their loved one is safe, comfortable, and living their richest, most joyful life possible.
At Memory Lane, this is exactly what we strive to provide every single day. We believe that even with cognitive challenges, every person deserves dignity, purpose, and connection. Our person-centered approach means we see beyond the diagnosis to the individual—their history, their preferences, their unique personality. We’re committed to being not just a care facility, but a true community where residents can flourish and families can breathe easier.
Your role doesn’t end when your loved one moves into long-term dementia care—it simply evolves. You remain a vital advocate, a cherished visitor, and an essential part of the care team. Together, we can ensure your loved one receives the quality care they deserve while you continue to be the family member they need, not the exhausted caregiver carrying an impossible burden alone.
Explore our specialized memory care services and find how Memory Lane can support your family through this important transition. We’re here to help, every step of the way.




